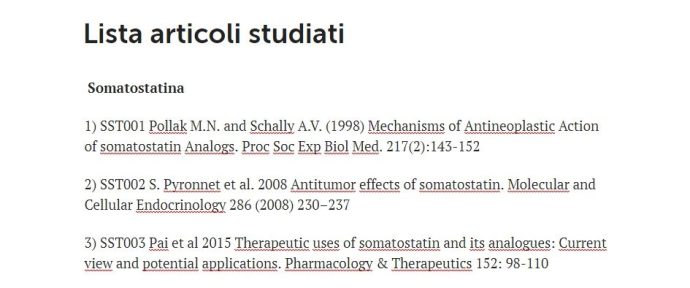
Lista articoli studiati
Somatostatina (SST)
1) SST001 Pollak M.N. and Schally A.V. (1998) Mechanisms of Antineoplastic Action of somatostatin Analogs. Proc Soc Exp Biol Med. 217(2):143-152. (link)
2) SST002 S. Pyronnet et al. (2008) Antitumor effects of somatostatin. Molecular and Cellular Endocrinology 286 (2008) 230–237. (link)
3) SST003 Pai et al (2015) Therapeutic uses of somatostatin and its analogues: Current view and potential applications. Pharmacology & Therapeutics 152: 98-110. (link)
4) SST004 Cascinu et al. (2014) Inhibition of Vascular Endothelial Growth Factor by Octreotide in Colorectal Cancer Patients. Cancer Investigation 19(1), 8–12. (link)
5) SST005 Danesi et al. (1997) Inhibition of Experimental Angiogenesis by the Somatostatin Analogue Octreotide Acetate (SMS 2O1-995). Clinical Cancer Research 3(2):265-72. (link)
6) SST006 Reubi and Laissue (1995) Multiple actions of somatostatin in neoplastic disease. Trends in Pharmacological Sciences 16 (3): 110-115. (link)
7) SST007 Schally A.V. (1998) Oncological Applications of Somatostatin Analogues. Cancer Research 48, 6977-6985. (link)
8) SST008 Schally A.V. et al. (1990) Antitumor effects of analogs of LHRH and somatostatin: experimental anche clinical studies. Journal of Steroid Biochemistry and Molecular Biology 37 (6): 1061-1067 (link)
Recettori della somatostatina (SSTr)
1) SSTr001 Zou Y., et al. (2019) Expression and selective activation of somatostatin receptor subtypes induces cell cycle arrest in cancer cells. Oncology Letters 17: 1723-1731 (link)
2) SSTr002 Priyadarshini et al. (2022) “Valutazione completa dei recettori della somatostatina in varie neoplasie: una revisione sistematica – Comprehensive Assessment of Somatostatin Receptors in Various Neoplasms: A Systematic Review.” Pharmaceutics, 14(7), 1394 (link)
GH (ormone della crescita) e GHRH (ormone di rilascio del GH)
1) GH001 Harvey (2010) Extrapituitary growth hormone. Endocrine 38:335–359. (link)
2) GH002 Subramani et al (2017) Role of Growth Hormone in Breast Cancer. Endocrinology 158(6):1543–1555. (link)
3) GH003 Subramani et al (2014) Growth hormone receptor inhibition decreases the growth and metastasis of pancreatic ductal adenocarcinoma. E xperimental & Molecular Medicine 46. (link)
4) GH004 Kaulsay et al (1999) Autocrine Stimulation of Human Mammary Carcinoma Cell Proliferation by Human Growth Hormone Experimental Cell Research 250, 35–50. (link)
5) GH005 Sustarsic at al. (2013) Human metastatic melanoma cell lines express high levels of growth hormone receptor and respond to GH treatment. Biochemical and Biophysical Research Communications 441(1):144-50. (link)
6) GH006 Kong et al (2016) Human growth hormone and human prolactin function as autocrine/paracrine promoters of progression of hepatocellular carcinoma. Oncotarget 7(20): 29465-79. (link)
7) GH007 Di Bella et al. (2018) The over-expression of GH/GHR in tumour tissues with respect to healthy ones confirms its oncogenic role and the consequent oncosuppressor role of its physiological inhibitor, somatostatin: a review of the literature. Neuroendocrinology Letters 39(4): 101-109. (link)
8) GH008 Basu R. and Kopchick J.J (2019) The effects of growth hormone on therapy resistance in cancer. Cancer Drug Resistance 2:827-846. (link)
9) GH009 Zhu et al. 2020 Growth hormone receptor promotes breast cancerprogression via the BRAF/MEK/ERK signaling pathway. FEBS Open Bio 10(6):1013-1020 (link)
10) GHRH01 Khanlari et al. (2018) “Espressione di GHRH-R, un biomarcatore potenzialmente bersaglio, nel carcinoma mammario triplo negativo – Expression of GHRH-R, a Potentially Targetable biomarker, in Triple-negative Breast Cancer”. Applied Immunohistochemistry and Molecular Morphology 26(1):1-5. (link)
11) GHRH02 Perez et al. (2012) “Gli antagonisti dell’ormone di rilascio dell’ormone della crescita sopprimono la crescita tumorale in vivo e l’espressione genica nei tumori al seno triplo negativi – Antagonists of growth hormone-releasing hormone suppress in vivo tumor growth and gene expression in triple negative breast cancers”. Oncotarget 3:988-997. (link)
12) GHRH03 Koster et al. (2009) “I tumori al seno triplo negativi esprimono recettori per l’ormone di rilascio dell’ormone della crescita (GHRH) e rispondono agli antagonisti del GHRH con l’inibizione della crescita” pubblicato sulla rivista Breast Cancer Research and Treatment è disponibile sul blog. (link)
Melatonina (MLT)
1) MLT001 Petronek et al. (2021) Utilization of redox modulating small molecules that selectively act as pro-oxidants in cancer cells to open a therapeutic window for improving cancer therapy. Redox Biology 42:101864. (link)
2) MLT002 Di Bella et al. (2013) Melatonin Anticancer Effects: Review. International Journal of Molecular Science 14, 2410-2430. (link)
3) MLT003 Kvietkauskas et al. (2020) The role of melatonin in colorectal cancer treatment: a comprehensive review. Therapeutic Advances in Medical Oncology 12: 1 –14. (link)
4) MLT004 Wang et al. (2019) Melatonin inhibits lung metastasis of gastric cancer in vivo. Biomedicine & Pharmacotherapy 117, 109018. (link)
5) MLT005 Chen et al. (2020) Melatonin suppresses epithelial to mesenchymal transition in the MG-63 cell line. Molecular Medicine Reports 21: 1356-1364. (link)
6) MLT006 Cheng et al. (2019) Melatonin restricts the viability and angiogenesis of vascular endothelial cells by suppressing HIF-1α/ROS/VEGF. International Journal of Molecular Medicine 43: 945-955. (link)
7) MLT007 Zharinov et al. (2020) Melatonin increases overall survival of prostate cancer patients with poor prognosis after combined hormone radiation treatment. Oncotarget, 11( 41): 3723-3729. (link)
8) MLT008 Maroufi et al. (2020) The potential therapeutic effects of melatonin on breast cancer: An invasion and metastasis inhibitor. Pathology – Research and Practice 216 (2020) 153226. (link)
9) MLT009 Liu et al. (2018) “Melatonin Inhibits Reactive Oxygen Species-Driven Proliferation, Epithelial-Mesenchymal Transition, and Vasculogenic mimicry in Oral Cancer”. Oxidative Medicine and Cellular Longevity, 3510970. (link)
10) MLT010 Fathizadeh et al. (2019) “Melatonin: an anti-tumor agent for osteosarcoma”. Cancer Cell International 19, 319 (link)
11) MLT011 de Godoy et al. (2023) “Azioni sinergiche di Alpelisib e Melatonina nelle linee cellulari di carcinoma mammario con mutazione del gene PIK3CA – Synergistic actions of Alpelisib and Melatonin in breast cancer cell lines with PIK3CA gene mutation”. Life Science 324, 121708. (link)
12) MLT012 Megerian et al. (2023) “Melatonina e cancro alla prostata: ruoli antitumorali e applicazione terapeutica – Melatonin and Prostate Cancer: Anti-tumor Roles and Therapeutic Application” Aging and Disease 14(3): 840-857 (link)
13) MLT013 Wang et al. (2022) “Uso della melatonina nei trattamenti antitumorali: a che punto siamo? – Use of Melatonin in Cancer Treatment: Where Are We?” International Journal of Molecular Science 23, 3779. (link)
14) MLT014 Fernández-Palanca et al. (2022) “Melatonina come agente antitumorale contro il cancro al fegato: una revisione aggiornata – Melatonin as an Antitumor Agent against Liver Cancer: An Updated Systematic Review.” Antioxidants 10(1), 103 (link)
15) MLT015 Di Bella et al. (1997) ““Melatonina con adenosina solubilizzata in acqua e stabilizzata con glicina per il trattamento oncologico: preparazione tecnica, efficacia e risultati clinici”. Neuroendocrinology Letters 2017; 38(7):465–474. (link)
16) MLT016 Kvetnoy et al. (1997) “Commentario: Il sistema neuroendocrino diffuso e la melatonina extrapineale – Commentary: The diffuse neuroendocrine system and extrapineal melatonin” Journal of Molecular Endocrinology 18, 1–3. (link)
17) MLT017 Kvetnoy (2002) “Melatonina extrapineale in patologia: nuove prospettive per la diagnosi, la prognosi e il trattamento della malattia – Extrapineal melatonin in pathology: New perspectives for diagnosis, prognosis and treatment of illness”. Neuroendocrinology Letters 23(Suppl 1): 92-96. (link)
18) MLT018 Kvetnoy et al. (2002) “La melatonina come pietra angolare della Neuroimmunoendocrinologia – Melatonin as the Cornerstone of Neuroimmunoendocrinology”. International Journal of Molecular Sciences 23(3), 1835. (link)
10) MLT019 Qadir et al. (2024) “Valutazione dei livelli di melatonina e antiossidanti nel siero di pazienti con cancro al seno – Evaluation of Melatonin and Antioxidant Levels in the Serum of Breast Cancer Patient”. BioMed Target Journal 2(1): 35-42. (link)
Prolattina (PRL)
1) PRL001 Costello (2019) “The Suppression of Prolactin is required for the Treatment of Advanced Prostate Cancer”. Oncogen 2:(3). (link)
2) PRL002 Levina et al. (2009) “Biological Significance of Prolactin in Gynecological Cancers” Cancer Research 69(12): 5226–5233. (link)
3) PRL003 Chou et al. (2021) “Regulation of extracellular and intracellular prolactin on cell proliferation and survival rate through GHR/JAK2/STAT3 pathway in NSCLC” Chemosphere 269:129625. (link)
4) PRL004 Sa-nguanraksa et al. (2020) “The role of Prolactin/Prolactin Receptor polymorphisms and expression in breast cancer susceptibility and outcome” Translational Cancer Research 9(10):6344-6353. (link)
5) PRL005 Sa-nguanraksa et al. (2021) “Expression of long-form prolactin receptor is associated with lower disease-free and overall survival in node-negative breast cancer patients». Gland Surgery 10(1):130-142. (link)
6) PRL006 Ding et al. (2017) “Autocrine Prolactin Stimulates Endometrial Carcinoma Growth and Metastasis and Reduces Sensitivity to Chemotherapy”. Endocrinology 158(6): 1595–1611. (link)
7) PRL007 da Silva et al. (2015) “Prolactin Promotes Breast Cancer Cell Migration through Actin Cytoskeleton Remodeling”. Frontiers in Endocrinology 6:186. (link)
8) PRL008 Kavarthapu et al. (2021) “Crosstalk between PRLR and EGFR/HER2 Signaling Pathways in Breast Cancer.” Cancers 2021: 13, 4685. (link)
9) PRL009 Fei et al. (2017) “Sex-related hormone receptor in laryngeal squamous cell carcinoma: correlation with androgen estrogen-ɑ and prolactin receptor expression and influence of prognosis”. Acta Oto-Laryngologica 138(1): 66-72. (link)
10) PRL010 Harbaum et al. (2010) “Clinicopathological significance of prolactin receptor expression in colorectal carcinoma and corresponding metastases”. Modern Pathology 23; 961-971. (link)
11) PRL011 Hathaway et al. (2021) “Prolactin and Risk of Epithelial Ovarian Cancer”. Cancer epidemiology, biomarkers & prevention 30(9):1652-1659. (link)
12) PRL012 Sethi et al. (2012) “Prolactin and cancer: Has the orphan finally found a home?” Indian Journal of Endocrinology and Metabolism16(Suppl 2): S195–S198. (link)
13) PRL013 Caponnetto et al. (2017) “Prolactin as a Potential Early Predictive Factor in Metastatic Non-Small Cell Lung Cancer Patients Treated with Nivolumab” Oncology 93(1):62-66. (link)
Mutagenesi (MUT)
1) MUT001 Lucien I. (1996) “Tumour Progression: Random Mutations or an Integrated Survival Response to Cellular Stress Conserved from Unicellular Organisms?” Journal of Theoretical Biology 178(4):375-380. (link)
2) MUT002 Michel B. (2005) “After 30 Years of Study, the Bacterial SOS Response Still Surprises Us”. PlosBiology 3(7):1174-1176. (link)
3) MUT003 Ben-Jacop et al. (2012) “Bacterial survival strategies suggest rethinking cancer cooperativity”. Trend in Microbiology 20(9):403-410. (link)
4) MUT004 Cipponi e Thomas (2014) “Stress-induced cellular adaptive strategies: Ancient evolutionarily conserved programs as new anticancer therapeutic targets”. Bioessays 36 (6): 552-560. (link)
5) MUT005 Li et al. (2021) “Non-Coding RNAs in Glioma Microenvironment and Angiogenesis”. Frontiers in Molecular Neuroscience 14. (link)
6) MUT006 Moore et al. (2021) “Exosomes in the Healthy and Malignant Bone Marrow Microenvironment”. In: Banerjee D., Tiwari R.K. (eds) Tumor Microenvironment: Cellular, Metabolic and Immunologic Interactions. Advances in Experimental Medicine and Biology, vol. 1350:67-89. Springer, Cham. (link)
7) MUT007 Matejka e Reindl (2019) “Perspectives of cellular communication through tunneling nanotubes in cancer cells and the connection to radiation effects”. Radiation Oncology 14, 218 (link)
8) MUT008 Kato et al. (2022) “La formazione di tunnel di nanotubi promuove la sopravvivenza contro il 5-fluorouracile nelle cellule di cancro al seno MCF-7 – Tunneling nanotube formation promotes survival against 5‐fluorouracil in MCF‐7 breast cancer cells”. Federation of European Biochemical Societies (FEBS) 12(1): 203–210 (link)
9) MUT009 Pasquier et al. (2013) “Il trasferimento preferenziale dei mitocondri dalle cellule endoteliali alle cellule tumorali attraverso nanotubi a tunnel modula la chemioresistenza – Preferential transfer of mitochondria from endothelial to cancer cells through tunneling nanotubes modulates chemoresistance”. Journal of Translational Medicine, 11:94. (link)
10) MUT010 Desir et al. (2018) “I tunnel di nanotubi indotti dalla chemioterapia mediano l’efflusso di farmaci intercellulari nel cancro del pancreas – Chemotherapy-Induced Tunneling Nanotubes Mediate Intercellular Drug Efflux in Pancreatic Cancer”. Scientific reports 21;8(1):9484 (link)
11) MUT011 Roehlecke e Schmidt (2020) “Tunnelling di nanotubi e microtubi tumorali nel cancro – Tunneling Nanotubes and Tumor Microtubes in Cancer”. Cancers, 12(4), 857 (link)
12) MUT012 Russo et al. (2019) “Mutabilità adattativa dei tumori del colon-retto in risposta a terapie mirate – Adaptive mutability of colorectal cancers in response to targeted therapies.” Science 366 (6472): 1473-1480. (link)
13) MUT013 Lambert et al. (2011) “Un’analogia tra l’evoluzione della resistenza ai farmaci nelle comunità batteriche e nei tessuti maligni – An analogy between the evolution of drug resistance in bacterial communities and malignant tissues”. Nature Reviews Cancer 11, 375–382. (link)
Pubblicazione di dati clinici del Metodo Di Bella (MDB)
1) MDB001 Di Bella et al. (2018) “Il sinergismo di somatostatina, melatonina, retinoidi, vitamin E, D3, C, inibitori prolattinici ed estrogenici, microdosi metronomiche di ciclofosfamide, ha incrementato sopravvivenza, risposte obiettive, performance status, in 297 casi di carcinomi del seno – The Synergism of Somatostatin, Melatonin, Vitamins Prolactin and Estrogen Inhibitors Increased Survival, Objective Response and Performance Status In 297 Cases of Breast Cancer”. Translational Biomedicine 9 No.1:146. (link)
2) MDB002 Di Bella et al. (2012) “Il Metodo Di Bella (MDB) ha migliorato sopravvivenza, la risposta obiettiva e il performance status in uno studio clinico osservazionale retrospettivo su 55 casi di linfomi – The Di Bella Method (MDB) improved survival, objective response and performance status in a retrospective observational clinical study on 55 cases of lymphomas”. Neuro Endocrinology Letters, 33(8):773-781 (link)
3) MDB003 Di Bella et al. (2013) “Il Metodo Di Bella (MDB) nel trattamento del cancro alla prostata: uno studio preliminare retrospettivo su 16 pazienti e una revisione della letteratura – The Di Bella Method (DBM) in the treatment of prostate cancer: a preliminary retrospective study of 16 patients and a review of the literature.” Neuroendocrinology Letters 34(6):523-528 (link)
4) MDB004 Di Bella et al. (2022) Di Bella et al. (2022) ” Uno studio osservazionale retrospettivo su casi di sarcoma trattati con il Metodo Di Bella: razionalità ed efficacia – A retrospective observational study on cases of sarcoma treated with the Di Bella Method: rationale and effectiveness.” World Journal of Pharmaceutical Research 11(7):1219-1278 (link)
5) MDB005 Di Bella et al. (2022) “Uno studio osservazionale retrospettivo sui casi di osteosarcomi trattati con una multiterapia: il razionale e l’efficacia – A retrospective observational study on cases of osteosarcomas treated with a multitherapy: The rationale and effectiveness.” Neuroendocrinology Letters 43(3): 173-179. (link)
6) MDB006 Di Bella et al. (2021) “Uno studio osservazionale retrospettivo su casi di tumori cerebrali anaplastici trattati con il Metodo Di Bella: razionale ed efficacia. – A retrospective observational study on cases of anaplastic brain tumors treated with the Di Bella Method: A rationale and effectiveness.” Neuroendocrinology letters 42(7):464–483. (link)
Retinoidi
1) RET001 Saffiotti et al. (1967) “Cancro sperimentale del polmone. Inibizione da parte della vitamina A dell’induzione della metaplasia squamosa tracheobronchiale e dei tumori a cellule squamose.” Cancer 20(5): 857-864 . (link)
2) RET002 Bollag W. (1979) “Retinoidi e cancro”. Cancer Chemotherapy and Pharmacology 3, 207–215. (link)
3) RET003 Strickland e Mahdavi (1978) “L’induzione della differenziazione nelle cellule staminali del teratocarcinoma da parte dell’acido retinoico – The Induction of Differentiation in Teratocarcinoma Stem Cells by Retinoic Acid” Cell 15: 393-403. (link)
4) RET004 Sporn (1977) “Retinoidi e Carcinogenesi – Retinoids and Carcinogenesis.” Nutrition Reviews, 35(4): 65–69. (link)
5) RET005 Sporn (1979) “Retinoidi e prevenzione del cancro – Retinoids and cancer prevention”. CA A Cancer Journal for Clinicians 29 (2): 120 – 125. (link)
6) RET006 Sporn (1976) “Approcci alla prevenzione del cancro epiteliale durante il periodo preneoplastico – Approaches to Prevention of Epithelial Cancer during the Preneoplastic Period.” Cancer Research 36: 2699-2702. (link)
7) RET007 Thein e Lotan (1982) “Sensibilità di cellule dell’osteosarcoma e condrosarcoma umano in coltura all’acido retinoico – Sensitivity of Cultured Human Osteosarcoma and Chondrosarcoma Cells to Retinoic Acid”. Cancer Research 42: 4771-4775 (link)
8) RET008 Welsch et al. (1980) “Effetto sinergico della soppressione cronica della prolattina e del trattamento con retinoidi nella profilassi della tumorigenesi mammaria indotta da N-metil-N-nitrosourea in cavie femmina Sprague Dawley – Synergistic Effect of Chronic Prolactin Suppression and Retinoid Treatment in the Prophylaxis of N-Methyl-N-nitrosourea induced Mammary Tumorigenesis in Female Sprague-DawleyRats.” Cancer Research 40(9): 3095-8. (link)
09) RET009 Nakajima et al. (1989) RET009 Nakajima et al. (1989) Inibizione da parte dell’acido retinoico della collagenolisi di tipo IV e dell’invasione attraverso una membrana basale ricostituita di cellule metastatiche di adenocarcinoma mammario di ratto – Inhibition by Retinoic Acid of Type IV Collagenolysis and Invasion through Reconstituted Basement Membrane by Metastatic Rat Mammary Adenocarcinoma Cells”. Cancer Research 49 (7): 1698–1706. (link)
10) RET010 Longnecker et al. (1982) “Inibizione della cancerogenesi pancreatica da parte dei retinoidi nei ratti trattati con azaserina – Inhibition of Pancreatic Carcinogenesis by Retinoids in Azaserine-treated Rats” Cancer Research 42:19-24. (link)
11) RET011 Mukherjee e Das (1990) “Azione antiproliferativa dell’acido retinoico nelle cellule tumorali cerebrali umane in coltura Gl-As-14(S) – Antiproliferative action of retinoic acid in cultured human brain tumor cells Gl-As-14(S)”. Cancer Letters 52(1):83-9. (link)
12) RET012 Schwartz e Shklar (1992) “L’effetto citotossico selettivo dei carotenoidi e dell’α-tocoferolo su linee cellulari tumorali umane in vitro – The Selective Cytotoxic Effect of Carotenoids and α-tocopherol on Human Cancer Cell Lines In Vitro.” Journal of Oral Maxillofacial Surgery 50:367-373. (link)
13) RET013 Kalemkerian et al. (1995) “Inibizione della crescita e induzione dell’apoptosi da parte del fenretinide nelle linee cellulari di cancro polmonare a piccole cellule – Growth Inhibition and Induction of Apoptosis by Fenretinide in Small-Cell Lung Cancer Cell Lines”. Journal of National Cancer Institute 87(22): 1674-1680. (link)
14) RET014 Zugmaier et al. (1996) “Effetti inibitori degli analoghi della vitamina D e dei retinoidi sulla crescita di cellule tumorali del pancreas umano – Growth inhibitory effects of vitamin D analogues and retinoids on human pancreatic cancer cells”. British Journal of Cancer 73: 1341-1346. (link)
15) RET015 Liu et al. (1996) “Il recettore dell’acido retinoico beta media l’effetto inibitorio della crescita dell’acido retinoico promuovendo l’apoptosi nelle cellule di cancro al seno umano – Retinoic acid receptor beta mediates the growth inhibitory effect of retinoic acid by promoting apoptosis in human breast cancer cells”. Molecular and Cellular Biology 16(3): 1138–1149. (link)
16) RET016 Mantellan et al. (2023) “Il recettore β dell’acido retinoico modula il meccanosensing e l’invasione nelle cellule tumorali del pancreas tramite la catena leggera della miosina 2 – Retinoic acid receptor β modulates mechanosensing and invasion in pancreatic cancer cells via myosin light chain 2”. Oncogenesis 12, 23 (link)
Acido ascorbico (vit. C)
1) ASC001 Stone (1984) “Cinquant’anni di ricerca sull’ascorbato e la genetica dello scorbuto: da una birra dal sapore migliore all’Homo Sapiens Ascorbicus – Fifty Years of Research on Ascorbate and the Genetics of Scurvy: From a Better Flavored Beer To Homo Sapiens Ascorbicus.” Journal of Orthomolecular Psychiatry 13(4): 280-284. (link)
2) ASC002 McCormick (1959) “Cancro: una malattia del collagene secondaria a una carenza nutrizionale? – Cancer: A Collagen Disease, Secondary to a Nutritional Deficiency?”. Archives of Pediatrics 76: 166-171. (link)
3) ASC003 Stone (1976) “La genetica dello scorbuto e il problema del cancro – The Genetics of Scurvy and the Cancer Problem”. Orthomolecular Psychiatry 5(3): 183-190. (link)
4) ASC004 Stone (1979) “Homo sapiens ascorbicus, un robusto mutante umano biochimicamente corretto – Homo sapiens ascorbicus, a biochemically corrected robust human mutant”. Medical Hypotheses 5(6):711-721. (link)
5) ASC005 Cameron et al. (1979) “Acido ascorbico e cancro: una revisione – Ascorbic Acid and Cancer: A Review”. Cancer Research 39(3): 663-681. (link)
6) ASC006 Mashauri (2023) “Scorbuto: una diagnosi differenziale trattabile, dimenticata e fatale, e una potenziale eziologia della leucemia e dell’anemia aplastica nella popolazione pediatrica.” Health Science Reports 6(10): e1611. (link)
7) ASC007 Lv et al. (2018) “La vitamina C uccide preferenzialmente le cellule staminali tumorali nel carcinoma epatocellulare tramite SVCT-2 – Vitamin C preferentially kills cancer stem cells in hepatocellular carcinoma via SVCT-2”. npj Precision Oncology 2:1. (link)
8) ASC008 Burgess et al. (2022) “L’aumento del contenuto di ascorbato nel glioblastoma è associato a una risposta ipossica soppressa e a una migliore sopravvivenza del paziente – Increased ascorbate content of glioblastoma is associated with a suppressed hypoxic response and improved patient survival. Frontiers in Oncology 12: 829524. (link)
9) ASC009 Cimmino et al. (2018) “Vitamina C nella riprogrammazione delle cellule staminali e nel cancro – Vitamin C in stem cell reprogramming and cancer” Trends in Cell Biology 28(9): 698-708 (link)
10) ASC010 Li et al. (2022) “Riposizionamento della vitamina C per il trattamento del cancro: il microambiente tumorale come bersaglio – Repurposing Vitamin C for Cancer Treatment: Focus on Targeting the Tumor Microenvironment”. Cancers 14(11), 2608 (link)
11) ASC011 Hickey e Roberts (2013) ” “Vitamina C e cancro: è utile la vitamina C orale? – Vitamin C and Cancer: Is There A Use For Oral Vitamin C?”. Journal of Orthomolecular Medicine 28(1), 33-44 (link)
12) ASC012 Gąbka et al. (2012) “Il potenziale elettrico di membrana e il pH intracellulare come fattori che influenzano la concentrazione intracellulare di ascorbato e il loro ruolo nel trattamento del cancro – The Membrane Electrical Potential and Intracellular pH as Factors Influencing Intracellular Ascorbate Concentration and Their Role in Cancer Treatment”. Cells 10(11), 2964. (link)
Vitamina D
1) VID001 Khamis et al. (2023) “Il triangolo magico nei disturbi orali potenzialmente maligni: vitamina D, il recettore della vitamina D e malignità – The Magic Triangle in Oral Potentially Malignant Disorders: Vitamin D, Vitamin D Receptor, and Malignancy.” International Journal of Molecular Science 24(20), 15058. (link)
2) VID002 Wu et al. (2018) “Riposizionamento della vitamina D per il trattamento delle neoplasie umane tramite il targeting del microambiente tumorale – Repurposing vitamin D for treatment of human malignancies via targeting tumor microenvironment” Acta Pharmaceutica Sinica B 6;9(2):203–219. (link)
3) VID003 Shan et al. (2020) “Analisi del trascrittoma: regolazione della staminalità del cancro nel carcinoma duttale mammario in situ da parte dei composti della vitamina D – Analysis of the Transcriptome: Regulation of Cancer Stemness in Breast Ductal Carcinoma In Situ by Vitamin D Compounds.” Cancer Prevention Research 13 (8): 673–686. (link)
4) VID004 Fernández-Barral et al. (2020) “Effetti della vitamina D sulla differenziazione cellulare e staminalità nel cancro – Vitamin D Effects on Cell Differentiation and Stemness in Cancer”. Cancer (Basel) 25;12(9):2413. (link)
5) VID005 “Il tsRNA-07804 mediato dalla vitamina D innesca la disfunzione mitocondriale e sopprime la progressione del cancro polmonare non a piccole cellule prendendo di mira il CRKL – Vitamin D-mediated tsRNA-07804 triggers mitochondrial dysfunction and suppresses non-small cell lung cancer progression by targeting CRKL”. Journal of Cancer Research and Clinical Oncology 150:51. (link)
Commenti disattivati